Beta lactamase-producing Neisseria gonorrhoeae alleviates Amoxicillin-induced chlamydial persistence
- David Ojcius
- Mar 30, 2023
- 5 min read
Highlights
• #Chlamydia trachomatis (CT) and $Neisseria gonorrhoeae (NG) co-infections are common.
• N. gonorrhoeae may cause a re-activation of persistent C. trachomatis infection.
• Transwell inserts eliminate contact-dependent NG anti-chlamydial effects in vitro.
• Penicillinase-producing NG alleviates Amoxicillin-induced chlamydial persistence.
Abstract
Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) cause most bacterial sexually transmitted infections (STIs) worldwide. Epidemiological studies have shown high percentages of co-infections with CT/NG and indicate that NG co-infection can reactivate CT shedding during persistent chlamydial infection. These data also suggest that biological interaction between the two bacteria may increase susceptibility or transmissibility. CT is an obligate intracellular bacterium with a developmental cycle that alternates between two forms: infectious elementary bodies (EBs) which invade the epithelium and non-infectious reticulate bodies (RBs) which divide and replicate inside the inclusion. Adverse environmental conditions can interrupt chlamydial development, with a consequent temporary halt in RB division, reduction in infectious EB production and formation of enlarged chlamydiae (aberrant bodies, ABs) – characterizing chlamydial persistence. When the stressor is removed, the chlamydial developmental cycle is restored, together with production of infectious EBs. The beta-lactam amoxicillin (AMX) induces chlamydial persistence, both in vitro and in mice. We investigated the impact of penicillinase-producing NG strain (PPNG) on AMX-persistent chlamydial infection utilizing our recently developed, contact-independent in vitro model of co-infection. We hypothesized that co-infection with PPNG could prevent and/or reverse AMX-induced chlamydial persistence. Our results showed that PPNG can ameliorate AMX-persistence in two chlamydial species, CT and C. muridarum (CM), providing novel evidence for a range of Chlamydia/NG interactions.
1. Introduction
Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) are the most prevalent bacterial sexually transmitted infections (STIs) worldwide, with an estimated 129 million new cases of chlamydia and 82 million new cases of gonorrhea in 2016, according to the World Health Organization (WHO). As Gram-negative obligate human pathogens, CT and NG primarily infect the epithelium of the endocervix in women and urethra in men leading to cervicitis and urethritis. Additional sites of infection for both pathogens are the rectum, pharynx and conjunctiva in both women and men (Leonard et al., 2019). Between 70–95% of women and 90% of men are commonly asymptomatic for CT, while 50% of women and 10% of men are asymptomatic for NG (CDC, NHS). If left untreated in women, both pathogens can spread to the upper reproductive tract, causing pelvic inflammatory disease (PID), which can result in persistent pelvic pain, ectopic pregnancy (EP) and infertility. Untreated infections in men can cause epididymitis and infertility (CDC, NHS).
CT is an obligate intracellular bacterium with a biphasic developmental cycle, consisting primarily of two bacterial forms: the infectious elementary body (EB) and the more metabolically active, but non-infectious reticulate body (RB). Chlamydial infection begins when the EBs adhere to and invade susceptible host cells; once the EBs are inside the cells, they are internalized in a membrane-bound vacuole called the inclusion. Inside the inclusion, the EBs differentiate into RBs which, largely utilizing host metabolites and energy, replicate and divide. After multiple cycles of replication, RBs differentiate again into EBs and are released into the extracellular environment to infect new host cells (AbdelRahman et al., 2016; Elwell et al., 2016). Diverse environmental conditions may cause divergence from the developmental cycle, leading the bacteria to enter a state referred to as persistence, or the chlamydial stress response. (Wyrick 2010; Bavoil 2014). Stressed chlamydiae, which are often atypical in appearance and thus called aberrant bodies (AB), are viable, but do not develop into EBs and therefore are not infectious.
Characteristically, upon removal of the stressor, persistent forms resume normal development and production of infectious EB. Persistence can be induced by nutrient (tryptophan or iron) deprivation, cytokine (Interferon gamma) exposure, monocyte infection by chlamydiae, viral co-infection of host cells, or penicillin exposure in vitro, the latter of which disrupts peptidoglycan synthesis and RB to EB differentiation (Schoborg 2011; Liechti et al., 2016). Amoxicillin (AMX), a commonly prescribed beta-lactam, induces chlamydial persistence in a murine infection model utilizing C. muridarum (CM) to model human CT vaginal infection (Phillips-Campbell et al., 2012). Additionally, mice with AMX-induced CM persistence subsequently treated with Azithromycin (AZM) had approximately twice the AZM treatment failure rate of productively infected mice, demonstrating that persistence can increase resistance to AZM in vivo, as well in vitro (Phillips-Campbell et al., 2014; Wyrick and Knight, 2004).
NG is a Gram-negative diplococcus which can adhere to host epithelial cells, typically replicating and forming microcolonies, and can also invade the host target cells. The adhesion and invasion mechanism are driven by NG surface structures, such as opacity (Opa) proteins, type IV pili, lipooligosaccharide (LOS) and the major outer membrane protein porin (PorB) (Quillin and Seifert, 2018). NG infection causes a rapid and robust recruitment of neutrophils (PMNs) to the site of infection, where NG is phagocytosed but capable of survival within the PMNs, and the resulting purulent exudate may facilitate transmission (Quillin and Seifert, 2018).
CT/NG co-infections are more common than can be explained by chance (Althaus et al., 2014), suggesting CT/NG interaction may play a role in transmission or infection. Furthermore, it has been suggested that N. gonorrhoeae may cause re-activation of latent or persistent CT infection (Richmond et al., 1972; Batteiger et al., 1989; Lin et al., 1998; Leonard et al., 2019). Nonetheless, in vitro and in vivo studies have focused on single-pathogen infections. To our knowledge, only three studies investigating CT/NG or CM/NG co-infection have been published in peer-reviewed journals, to date. The first study, an in vivo CM/NG mouse vaginal co-infection study, showed increased vaginal viable NG recovery and PMN induction in CM/NG co-infected mice compared to NG single infected mice (Vonck et al., 2011). The second study, utilizing, in part, a CT/NG ex vivo human co-infection model showed that CT infection of PMNs reduced neutrophil extracellular trap (NET) formation and NG killing upon subsequent exposure of the PMN to NG (Rajeeve et al., 2018). Finally, the third study using a CT/NG in vitro co-infection model recently developed in our laboratory, showed that direct contact of NG with CT, in the setting of a genital epithelial host cell line, caused an anti-chlamydial effect (Onorini et al., 2022). The three studies together, demonstrated interplay between CT and NG, in vitro and in vivo, during productive chlamydial infection.
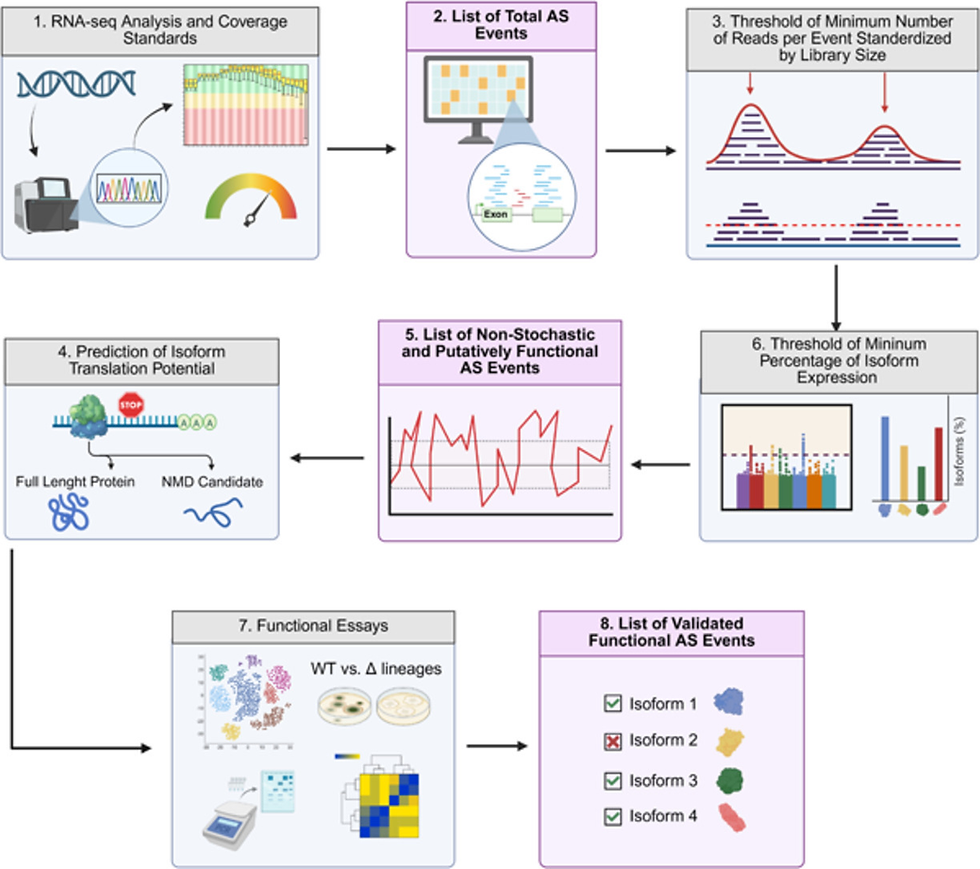
Given that clinical studies suggest specifically that NG co-infection may re-activate persistent, undetected chlamydial infection (Batteiger et al., 1989; Lin et al., 1998), we aimed to evaluate the impact of penicillinase-producing NG (PPNG) on AMX-persistent chlamydial infection. We hypothesized that PPNG co-infection, either at the time of chlamydial infection or after chlamydial infection, would alleviate chlamydial persistence caused by AMX. Because our existing in vitro co-infection model caused a marked anti-chlamydial effect upon direct NG contact of CT host cells (Onorini et al., 2022), we established a new contact-independent in vitro model of co-infection. In this model, we used transwell inserts to prevent this NG anti-chlamydial effect, allowing us to effectively address our hypothesis. The inserts allowed PPNG-secreted substances, such as penicillinase, into the shared culture medium while preventing the NG contact-dependent anti-chlamydial effect observed in the previous study. Our results showed that PPNG can both prevent and largely reverse AMX-induced chlamydial persistence. Importantly, this novel CT/NG co-infection model is a useful research tool, potentially contributing to the currently limited understanding of CT/NG interactions in the context of modeled epithelial infection.
Free article. Read more at:














Comments