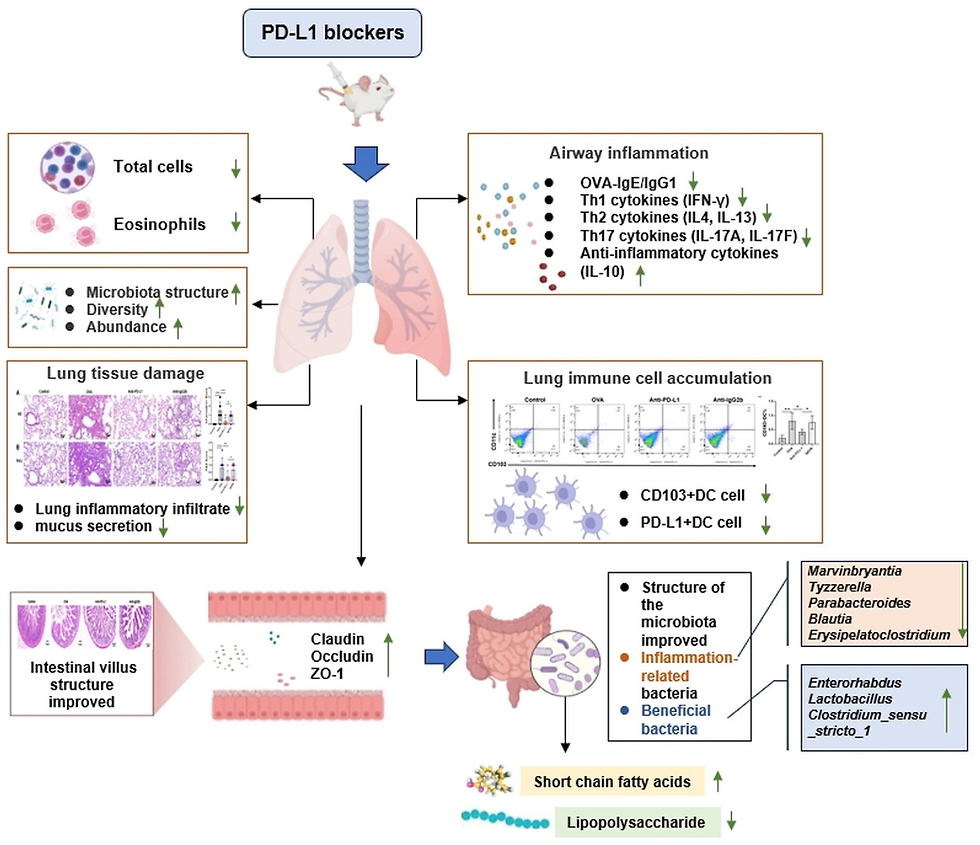
Anti-PD-L1 improves barrier function and reduces CD103+ DC cell accumulation by regulating gut and lung microbiota and its metabolites to alleviate asthma in juvenile mice
- David Ojcius
- 48 minutes ago
- 2 min read
Highlights
PD-L1 blockade can restore the Th1/Th2/Th17 balance.
The intestinal barrier function was improved after PD-L1 blockade.
PD-L1 blockade can induce the downregulation of CD103+ DCs.
PD-L1 blockade improves microbiota composition, increases Lactobacillus and SCFAs in feces, and reduces LPS in BALF.
Abstract
Background
Programmed death ligand 1 (PD-L1) was found to play an important role in maintaining tolerance and immune balance, and its mechanism of action on asthma still needs to be further clarified.
Material and methods
in a juvenile asthma model, PD-L1 blockers were used to inhibit the expression of PD-L1 in vivo. By evaluating parameters that reflect airway hyperresponsiveness, airway inflammation, tissue damage, intestinal barrier function, and microbiome changes in mice, the impact of PD-L1 blockade on various physiological and immune indicators in asthma models is fully revealed.
Results
PD-L1 blockade reduces leukocyte infiltration in the lungs, including eosinophils, decreased levels of IgE and IgG1, and restored Th1/Th2 imbalance by reducing IL-4, IL-13, and GATA-3 while increasing IFN-γ. In addition, PD-L1 blockade significantly decreased levels of IL-17A/F and increased IL-10. Histological analysis of the lungs showed that PD-L1 blockade attenuated airway inflammatory cell infiltration and mucus hyperproduction. Further testing showed that the intestinal barrier function was improved after PD-L1 blockade. Mechanistic studies revealed that PD-L1 blockade improved microbiota composition in the lungs and gut, increased Lactobacillus, SCFA, and reduced LPS. As well as induced the downregulation of CD103+ DCs in lung. Correlation analysis showed that airway inflammation is negatively correlated with SCFA and positively correlated with LPS, and barrier function is negatively correlated with LPS.
Conclusions
PD-L1 blockade alleviated asthmatic airway inflammation by modulating gut and lung microbiota, improving intestinal barrier function, increasing SCFA levels, reducing LPS and CD103+ DCs activity.
Read full article for free (open access):












Comments